Six year old Charlotte is a total diva. She loves fashion, dancing and wants to be a popstar when she grows up. She is super affectionate and so incredibly smart and intuitive beyond her years. Charlotte also lives with a rare health condition.
We first noticed that something wasn’t quite right with Charlotte when she was six weeks old. She wasn’t digesting her milk well and she slept a lot. Our midwife and then Plunket nurse were both concerned enough to tell us to get her to hospital to be checked out.
Our concerns were put aside when the hospital assured us that she was OK. Being first time parents, we were told we were probably over reacting. We would continue to hear this same story over the next 12 months. Meanwhile Charlotte became sicker and we would often struggle to wake her.
Hospitalisations became so frequent that at times we would only get home for 10 days before having to be admitted again. The first night Charlotte lost consciousness and had a hypoglycaemic coma event we refused to leave hospital without answers and begged doctors to work out what was wrong.
Searching for answers
Charlotte had a lot of different symptoms and test results that didn’t tick boxes or paint a clear picture. She was often treated for the presenting issue and discharged without knowing what was causing it.
We went private and searched for doctors we thought may be able to look deeper into Charlotte’s condition. We were lucky to get a supportive Paediatrician and GP. They were so perplexed by Charlotte and knew that although the dots didn’t connect, it didn’t mean there wasn’t an underlying reason behind them. With their help we got in front of the National Metabolic team at Starship. The team agreed that Charlotte did not tick boxes and the risks to her life and brain function warranted a trip to Starship to investigate.
A rare metabolic defect
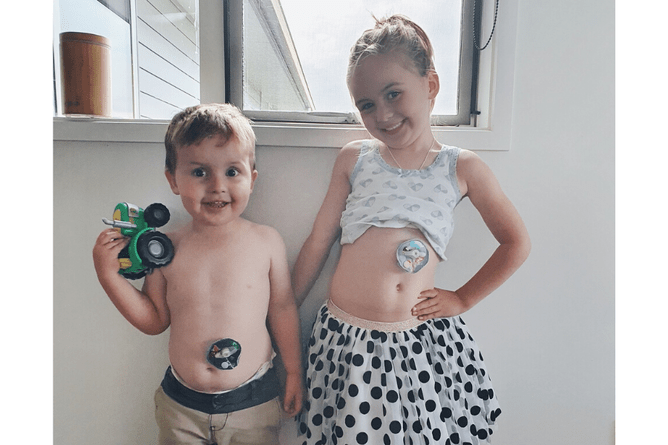
Today, three years down the track we still don’t have a name for Charlotte’s condition. She has a rare metabolic condition, one that the Starship team had not seen in any other child in NZ. That is until 2017, when approaching his first birthday, her younger brother Lachlan started presenting with the same symptoms as Charlotte.
The condition means their bodies are unable to process ketones correctly and therefore do not convert energy from food efficiently. They are always in ketosis even when fully fed, which means they cannot fast for any period of time. With any fasting more than four hours they tend to go hypoglycaemic very quickly and with often no distinct signs until we can’t wake them.
When they have any added stress on their body like a common cold, their body cannot meet the additional energy requirements. They require hospitalisation for port access to administer IV dextrose – and even then this often takes days to correct. Charlotte and Lachlan eat regularly with special diets and high calorie meal replacers. They have a high glucose solution pump fed through their gastrostomy for any extended period of fasting (overnight, or fasting for surgery).
The risks to them if we don’t manage them closely? Brain damage from recurrent low blood sugars, as well as coma and if it were not rectifiable this would lead to death. The pressures on their bodies have thrown other medical issues along the way like malabsorption and fat soluble vitamin deficiencies.
Living with a rare condition
Our family is probably quite different to many, but it has become our new normal.
Enteral nutrition (tube feeding) and constant monitoring have become second nature to us. We can spot a hospitalisation coming from the smell of their breath (Ketosis has a very unique smell!)
Having children with a rare condition is challenging, frustrating, hard and isolating.
When a child’s condition is rare, it is hard for people to understand what it is, including senior doctors and consultants, let alone education and support services etc.
The team at Starship have taken on their care and management, and have been an amazing support to our family. With the plans they have implemented we are able to care for both children at home, and our time as inpatients has diminished substantially.
Getting genetic testing has been a slow process. I am glad to say now that after six years of Charlotte being ill, they are in a genetic study to try and identify the gene responsible.
In the early days Charlotte’s care wasn’t looked at with a long-term view because no one knew what was going on or why. The procedures undertaken often left Charlotte traumatised. She didn’t have things like play therapy and sedation to help her cope with what she was going through.
As a result, she has understandably developed procedural anxiety and now requires sedation for almost all interventions. She also suffers from separation anxiety. Starting school recently has highlighted the fact that she is “different” with ports and tubes. This has been another hurdle for her self-confidence.
True Colours
True Colours came in to our lives when we moved to the Waikato region nine months ago. Charlotte’s worries were stopping her from partaking in everyday activities.True Colours gives Charlotte a safe and fun environment to address her worries rather than another hospital setting. Our counsellor Kyra Lindsey has quickly formed a good relationship with Charlotte. She always looks forward to a “Kyra day.”
The resources and knowledge pool available to us from True Colours gives us the ability to try and tackle issues at home as well. It has also been a huge help to Charlottes confidence to know that she is not alone. That there are other children out there facing similar issues to her. As Lachlan gets older and can voice his feelings I have no doubt that True Colours will help him in the same ways.
Thanks to the Smith family for sharing their story with us